Authors: M. Ginjaume1, E. Carinou2, F. Vanhavere3, G. Gualdrini4, I. Clairand5, M. Sans Merce6
1 Institute of Energy Technologies, Universitat Politècnica de Catalunya (UPS), Spain
2 Greek Atomic Energy Commission (GAEC), Greece
3 Belgian Nuclear Research Centre (SCK-CEN), Belgium
4 Radiation Protection Institute - Ente per le Nuove Tecnologie LEnergia et lAmbiante (ENEA), Italy
5 Institut de Radioprotection et de Sûreté Nucléaire (IRSN), France
6 University Hospital Center Vaudois (UPC), Switzerland
The CONRAD project, funded by the EU within FP6 from 2004 to 2007, aimed to coordinate research on radiation protection in the workplace. One of the working groups in the network highlighted high extremity doses and a lack of systematic data analysis on exposures to staff in interventional radiology and nuclear medicine [1]. To improve the standards for protection of medical staff for procedures that may result in high exposures, a project called ORAMED Optimization of Radiation Protection of Medical Staff, was launched in 2008 within the framework of EURATOM FP7. ORAMED focuses on having better knowledge of extremity and eye lens exposures and developing new technologies for eye-lens measurement and for active personal dosemeters to be used in pulsed fields.
Ten Institutes, Belgian Nuclear Research Centre (Belgium), Commissariat à lEnergie Atomique (France), ENEA Radiation Protection Institute (Italy), Federal Office for Radiation Protection (Germany), Greek Atomic Energy Commission (Greece), Institute for Radiological Protection and Nuclear Safety (France), Nofer Institute of Occupational Medicine (Poland), Slovak Medical University (Slovakia), Universitat Politècnica de Catalunya (Spain), University Hospital Centre Vaudois (Switzerland) and two enterprises, MGP Instruments (France) and RADCARD (Poland), are taking part in the project. The activities are divided into 5 Work-Packages:
- optimization of radiation protection in interventional radiology,
- development of practical eye lens dosimetry in interventional radiology,
- optimization of the use of active personal dosemeters in interventional radiology,
- improvements in extremity dosimetry in nuclear medicine, with special emphasis for PET applications and nuclear medicine therapy, and
- knowledge dissemination and training.
The project is to be finished in February 2011, thus the activities are still under progress. A summary of the main objectives and activities developed until now by the different work-packages are described in this paper.
1. Optimization of radiation protection in interventional radiology
An extensive campaign of measurements and Monte Carlo calculations of extremity and eye lens doses in interventional radiology is in progress to obtain a set of standardized data on doses to staff in interventional radiology and cardiology and to design recommended radiation protection measures in order to optimize staff protection.
Figure 1 shows an image of the geometry and mathematical phantoms used for the simulation of the patient and physician during an interventional radiological procedure.
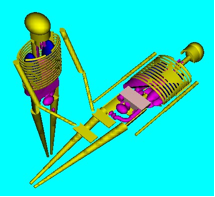
Figure 1. Mathematical phantoms and geometry used for MC simulation of interventional radiology procedures
So far, more than 660 procedures from 22 European hospitals have been analyzed. The monitored procedures are divided into three main categories: cardiac procedures; general angiography procedures; and endoscopic retrograde cholangiopancreatography procedures (ERCP). The eyes, wrists, fingers and legs of physicians are monitored and measured doses are correlated with radiological parameters such as the tube voltage and the air-kerma area product. The highest doses are often found in the left monitored finger but many parameters, such as, the availability and use of protective equipment (lead-glasses, mobile shields), tube position (above or below the table), access (femoral or radial) and a number of other procedure characteristics (use of cine/fluoro, beam projections etc) are found to influence the extremity and eye lens doses. A significant dose reduction is observed when the tube is below the table and/or when shielding is used. Finally, it should be mentioned that the examples of bad practices encountered during monitoring of the above procedures (hands inside the beam, improper use of additional protective equipment) strongly indicate the need for radiation protection training of the medical staff.
2. Development of practical eye lens dosimetry in interventional radiology
Increased evidence of radiation-related lens opacities in interventional radiologists has been reported in recent years [2]. However, the eye lens doses are never measured in routine procedures and, at the present time, there is a lack of methods to measure such doses. At the moment, a protocol to calculate and reproduce the operational quantity, personal dose equivalent at a depth of 3 mm of tissue, Hp(3,α), in calibration laboratories has been developed and a set of conversion coefficients from air kerma to Hp(3,α) has been proposed [3]. In addition, on the basis of the computed quantities, a dosemeter prototype, optimized to respond in terms of Hp(3) is under development by RADCARD. Figure 2 shows one of the prototypes. The overall procedure is also supported with type test irradiations carried out at the Laboratoire National Henri Becquerel, CEA Saclay.

Figure 2. Eye-lens dosemeter
3. Optimization of the use of active personal dosemeters in interventional radiology
Active personal dosemeters (APD) have been found to be very efficient tools to measure occupational doses in many applications of ionizing radiation. However, their use for interventional radiology cannot be generalized. The behaviour of 7 commercial APD models, deemed suitable for application in interventional radiology, has been analyzed through several tests under laboratory conditions with reference continuous and pulsed X-ray beams. Figure 3 presents a photograph of the tested APDs.


Figure 3. APDs tested in ORAMED
Most tested APDs present a satisfactory response at low photon energies, down to 24 keV, which is sufficient for interventional radiology. However, some of them do not fulfil the ISO 61526 standard requirements [4] concerning dose rate and angular response. Tests in pulsed mode show that the limitations of several APDs are mostly due to high dose-rates rather than to pulse frequency. This point was confirmed by tests in hospitals. These results have identified those devices that can provide useful indications of personal doses during interventional procedures, and those that should not be used in this field. The development of a new prototype that would overcome the present limitations of the APDs is being undertaken by MGP Instruments.
4. Improvements in extremity dosimetry in nuclear medicine, with special emphasis for PET applications and nuclear medicine therapy
Extremity doses in nuclear medicine, especially in therapy, can be very high if adequate radiation protection measures are not followed. As in the case of interventional radiology, a European campaign of extremity measurements in nuclear medicine departments is in progress. The doses to the different parts of the hands have been systematically mapped in more than 100 workers from 31 nuclear medicine departments, with special attention paid to 90Y unsealed therapy sources. Special gloves have been designed to measure the hand dose on 11 different points of the hand. Figure 4 illustrates the procedure of radiopharmaceutical administration in nuclear medicine. The technician of the photograph is wearing the ORAMED special gloves to monitor the distribution of dose in the hands.

Figure 4. Radiopharmaceutical administration in nuclear medicine
Monte Carlo simulations are simultaneously performed to determine the main parameters that influence the hand dose distribution and the effectiveness of different radiation protection measures.
Preliminary results show large variations of skin doses across the hands depending on the radionuclide and the procedure, but also large differences are found between technicians. In some cases, skin dose equivalent limit could be exceeded. The final analysis of the results should provide information on the real doses to nuclear medicine workers and help to identify the best practices in this field.
5. Knowledge dissemination and training
The training material which is being prepared within the framework of ORAMED will aim to give a practical understanding on how to improve radiation protection practice in some medical applications where, at present, doses are potentially high. The problems analyzed are, in general, not included in most available training courses for medical staff. The training material will improve actual education information. The contacts and collaboration with professional societies and international organizations should enable widespread dissemination of the material.
Along these lines, ORAMED members are involved in the recently created Medical ALARA network (EMAN), which has as main objective the establishment of a sustainable network where different stakeholders within the medical sector will have the opportunity to discuss and to exchange information on different topics related to the implementation of the ALARA principle in the medical field.
In addition, in January 2011, an international workshop to present the main results of the ORAMED project will be organized in Barcelona. Round tables with the identified stakeholders will be programmed to promote good discussion and feedback of the results. The e-learning modules will be presented on this occasion and made available to collaborating professional organizations and interested institutions in the field.
For more information, you are invited to visit the ORAMED web-site www.ORAMED-fp7.eu.
References
[1] Vanhavere, F.; Carinou, E.; Donadille, L.; Ginjaume, M.; Jankowski, J.; Rimpler, A.; Merce, M. S.; An overview on extremity dosimetry in medical applications. Radiat Prot. Dosim. 129: 350-355, 2008
[2] Vañó, E.; González, L.; Beneytez, F.; and Moreno, F. Lens injuries induced by occupational exposure in non-optimized interventional radiology laboratories. Br. J. Radiol. 71: 728-733; 1998.
[3] Mariotti, F.; Gualdrini, G. ORAMED Project. Eye-lens dosimetry. A new Monte Carlo approach to define the operational quantity Hp(3), ISSN/0393-3016, RT/2009/1/BAS.
[4] International Electrotechnical Commission. Radiation protection instrumentation. Measurement of personal dose equivalent Hp(10) and Hp(0.07) for X, gamma, neutron and beta radiation: Direct reading personal dose equivalent and/or dose equivalent rate dosemeters (1998) IEC 61526 Geneva: IEC
Acknowledgements
The research leading to these results has received funding from the European Atomic Energy Community's Seventh Framework Programme (FP7/2007-2011) under grant agreement n° 211361.
