E.G. Friberg, A. Widmark, M. Solberg, T. Wøhni, G. Saxebøl
Section for Dosimtery and Medical Applications, Norwegian Radiation Protection Authority (NRPA), Norway
Introduction
C-arms are a common tool in many interventional and surgical procedures performed outside radiological departments. Common for these procedures is that the C-arm often is operated by physicians without any formal education and training in radiation protection. Modern C-arms have now become highly technically advanced, are used in more and more complex and time consuming procedures and have the potential to deliver high patient doses if operated by unskilled persons. To overcome this problem the Medical Exposure Directive (MED) states in article 7 that radiation protection should be implemented in the basic education for physicians [1]. Norway, as a non-member of the European Union, has not implemented this requirement and radiation protection is practically absent in the basic curriculum of Norwegian medical schools. Our national radiation protection regulation from 2004 states however, that all Hospital Trusts (HT) are obliged to ensure that all personnel involved in radiological examinations have sufficient qualifications and skills in radiation protection [2]. In addition, all HTs must be authorized by the Norwegian Radiation Protection Authority (NRPA) in order to use advanced X-ray equipment for medical purposes. During the authorization process, 54% of the HTs reported inadequate skills in radiation protection among personnel involved in radiological examinations at their local hospitals. The lack of skills in radiation protection was mainly associated with physicians and nurses who were involved in the use of mobile C-arms outside the radiological departments. Finally all HTs confirmed that they had an operating system to ensure that all personnel involved in radiological examinations have sufficient qualifications and skills in radiation protection. The aim of this work was to verify through inspections whether the HTs self-declared compliance regarding training and skills in radiation protection were sufficient or not.

Material and method
The public health care system in Norway is administrated under the Ministry of Health and Care Services. There are approximately 70 public hospitals organized in 21 Hospital Trusts (HT) located under four regional Health Authorities (HA). The NRPA carried out inspections at 52% of all HTs during the year 2008 and 2009. HTs from all regional HAs were included, covering a total of 26% of all the Norwegian public hospitals. The inspections were a direct follow-up of the authorization given to the HTs, with special focus on education and training in radiation protection outside the radiological department. The inspections were carried out as quality system audits, based on document reviews, interviews, on-site inspections and verifications. The HTs local procedures for education and training in radiation protection were reviewed in advance of the inspection. On-site interviews included staff having personnel management and physicians and nurses who were involved in X-ray guided procedures using C-arms. To verify if all involved staff had received training in radiation protection, spot checks of the departments documentation of training were asked for and reviewed.
Results
Procedures for education and training in radiation protection were received from only 64% of the inspected HTs. A review of the procedures indicated that the responsibility for staff involved in X-ray guided procedures was placed on the department heads. All procedures covered regular training in general radiation protection and equipment specific training, including requirements for records of training courses, preferably by signed lists of attendance. Interviews with the department heads revealed that many of them were unaware of their responsibility, some were also unfamiliar with the existence of the procedure in general. A clear distinction between the levels of awareness in radiation protection was observed between nurses and physicians, nurses having the highest level of awareness. Most HTs did not have a systematic approach for education and training in radiation protection. Courses in radiation protection were occasionally held by the radiation protection officer or a medical physicist. The level of attendance on these courses varied between the different professionals (physicians and nurses), departments and hospitals within each HT. Existing systems for documentation of education and training (if any) were highly insufficient at all HTs.
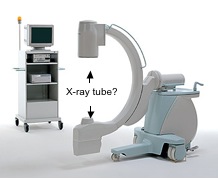
Interviews also revealed some serious lack of skills in radiation protection. Typical examples were: unable to identify the X-ray tube from the image intensifier of the C-arm, inadequate knowledge of the operating consol, no knowledge of the three cardinal principles for staff protection (time, distance and shielding), no deliberate use of collimation and/or pulsed fluoroscopy, and total lack of knowledge about patient doses and risks. In many HTs nurses assisted the physicians by operating the C-arm console. For those cases it was not uncommon to just switch on the X-ray unit and start to fluoroscopy regardless of the default exposure settings on the consol.
The inspections performed by NRPA concluded that 91% of the inspected HTs had non-conformities with the requirements regarding skills and training in radiation protection. This finding makes the HTs self -eclared compliances with the regulation highly questionable.
Discussion and conclusion
The lack of skills in radiation protection among personnel outside radiological departments is clearly not a fiction. The main reason for this is that most HTs had an insufficient system for systematic and frequent education and training in radiation protection. Also the fact that responsible persons were unaware their responsibilities and a general lack of involvement and focus on radiation protection outside radiological departments have to be considered. The lack of knowledge about doses and risks among leaders often tends to unconsciously undermine the importance of radiation protection. As a consequence, radiation protection is often ignored or not prioritized, even though the responsibility is clearly defined.
With modern C-arms becoming more and more complex with the possibility to give high patient doses if operated by unskilled persons, the observations from Norwegian hospitals give rise to concern. There is an urgent need for increasing the knowledge of patient doses and risks among physicians and nurses. The most efficient way to overcome this situation is by introducing radiation protection in the basic education of physicians as stated in the MED. In the short term, focus should be on developing functional systems for education and training in radiation protection locally at each HT and introducing personal driving licenses for operating C-arms. Finally, the biggest challenge is to overcome the bad attitude towards radiation protection present among some physicians. Teaching some dos and donts can have a tremendously impact on patient doses, especially if competence in radiation protection is totally absent [3]. To conclude, there is a common responsibility of the community to improve the operators skills in radiation protection and in this way try to prevent radiation induced hazards caused by malpractice.
References
[1] Council Directive 97/43/EURATOM on health protection of individuals against the dangers of ionising radiation in relation to medical exposure. Official Journal L-180, 09.07.97, p. 22-27.
[2] Regulations No. 1362 of 21 November on Radiation Protection and Use of Radiation (Radiation Protection Regulations). Oslo, 2003. http://www.nrpa.no/archive/Internett/Publikasjoner/Annet/act_eng.pdf (17.02.2010).
[3] Widmark A, Friberg EG. How dos and donts can be of significant importance in radiation protection training. In: 4th International Conference on Education and Training in Radiological Protection, Lisbon 2009. ETRAP 2009 transactions. Poster session. Brussel: European Nuclear Society, 2009. http://www.euronuclear.org/events/etrap/transactions/ETRAP09-poster.pdf (17.02.2010)
